For the childhood cancer community
Children with cancer deserve more. We’re on a mission to bring greater awareness, funding, and hope to pediatric cancer—and we invite you to be part of it. Discover our “Why” and how we can stand together for change.
❊ Preview our work
Creating hope in every childhood battle.
Childhood Cancer Awareness
September is Childhood Cancer Awareness Month, a time to shine a light on the 15,000 children diagnosed each year in the US. It's more than gold ribbons; it's about amplifying voices, driving research, and supporting families in the fight for a brighter future.
Read our FAQ below for more facts.
Toy Drives
Our biannual toy drives bring joy and comfort to children battling cancer at Children's National and elsewhere. With over 2,000 toys donated since 2024 and an Amazon wish list open year-round, each gift reminds these brave children that they are not alone.
Initiatives coming soon!
We are building beyond the present: expanding advocacy and awareness, improving support services for patients and families, with a special focus on Spanish-speaking families, and forging alliances with local and national childhood cancer organizations. Together, we are creating a stronger, more inclusive support network for every child and family.
For example, our Director of Policy and Advocacy (Maria Casoni) is also a member of CURE Childhood Cancer’s Young Professional Leadership Council (YPLC). Read more about YPLC here.
❊ News
Looking for support? Search The Childhood Cancer Hub
The Childhood Cancer Hub is a community-driven directory of organizations, including LIVS Creative Legacy, that support children and teens with cancer, survivors, and their families, maintained by the Coalition Against Childhood Cancer.
❊ Childhood Cancer FAQs
Childhood Cancer Facts
-
It generally refers to cancers diagnosed in children and adolescents under the age of 20.
“One in 264 children & adolescents is estimated to be diagnosed with cancer before the age of 20 years.” Source: CAC2
-
“The average age at diagnosis is 10 overall (ages 0 to 19), 6 years old for children (aged 0 to 14), and 17 years old for adolescents (aged 15 to 19).”
“Leukemia is the most common childhood cancer (ages 0-14), accounting for 28% of cases, followed closely by central nervous system tumors (27%), one-third of which are benign or borderline malignant.”
“In 2025, an estimated 9550 children (aged birth to 14 years) and 5140 adolescents (aged 15–19 years) will be diagnosed with cancer.”
“Approximately 5.7% of newly diagnosed brain tumors, including adults, occur under age 20.”
Source: CAC2
-
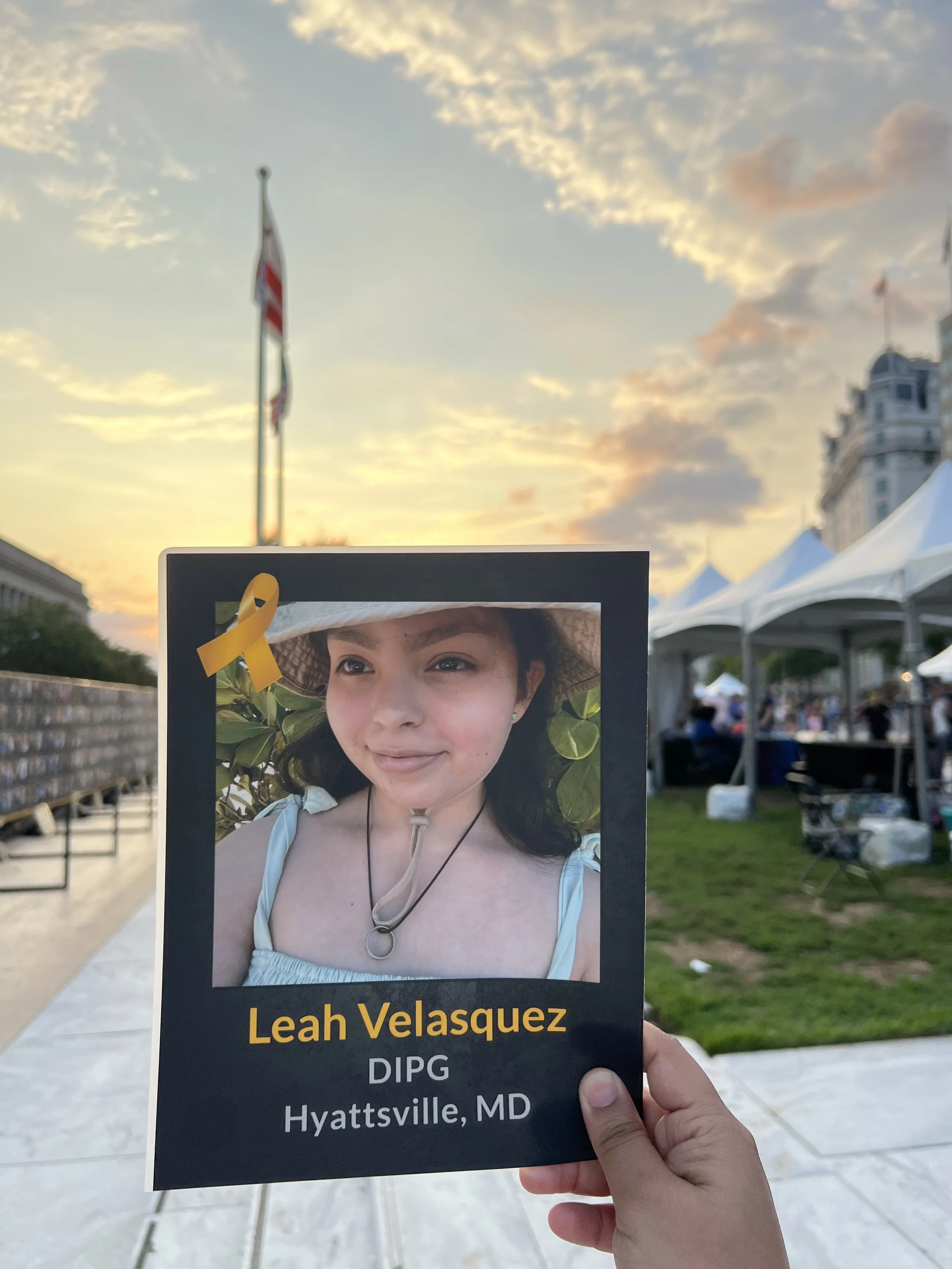
“Cancer survival rates vary not only depending on the type of cancer, but also on individual factors attributable to each child. Five-year survival rates can range from almost 0% for cancers such as DIPG (2.2%), a type of brain cancer, to over 90% for the most common type of childhood cancer known as Acute Lymphoma Leukemia (ALL).
Diffuse Intrinsic Pontine Glioma (DIPG) represents approximately 80% of the malignant brainstem tumors occurring in children. In the United States, about 300 children are diagnosed with DIPG each year. DIPG primarily affects children between the ages of 5 and 10 years but can occur in younger children and teens. DIPG is rare in adults.
Despite numerous clinical trials, outcomes of children with DIPG continues to remain dismal, with a median survival of only 11 months, while only 10% of DIPG patients have a ≥ 2-year overall survival (OS) rate.”
Source: CAC2
-
Cancer survival rates vary not only depending on the type of cancer, but also on individual factors attributable to each child. Cancer treatments may harm the body's organs, tissues, or bones and cause health problems later in life. They may include physical, mental, and social problems and second cancers. These health problems are called late effects as a result of surgery, chemotherapy, radiation therapy, and/or stem cell transplant. Late effects in childhood cancer survivors affect the body and mind. Late effects may affect organs, tissues, body function, growth and development. Other late affects are mood, feelings and actions thinking, learning, and memory as well as social and psychological adjustment. Late effects also have a risk of second cancer.
Source: CAC2
-
Affordability: Survivors often face significant financial strain. Compared to peers with no cancer history, they are more likely to struggle with medical bills and delay care. Treatment-related work disruptions can force families to lose substantial income, and many survivors already live in or near poverty at diagnosis.
Knowledge: Both survivors and healthcare providers may lack information about the need for long-term monitoring and guidelines for appropriate follow-up. Survivors treated at very young ages may not be fully aware of risks, and some providers are not trained on survivorship guidelines. This knowledge gap affects access to essential care such as psychosocial and palliative services.
Proximity: Survivorship clinics are often located far from where survivors live, especially those with limited financial resources. Travel requirements create an additional barrier, making it harder to adhere to recommended monitoring.
The stakes are high: childhood cancer survivors remain at risk for serious late effects—including heart conditions, developmental problems, and new cancers—yet fewer than one-third follow surveillance guidelines for key risks like cardiac, thyroid, and breast health. Without targeted interventions to address affordability, knowledge, and proximity, these survivors face preventable health challenges that extend long after their initial treatment.
Source: CAC2
-
Federal funding for childhood cancer research in the U.S. is spread across several programs, with specific recent initiatives and amounts shedding light on the overall investment. Key points include:
The National Cancer Institute (NCI) has a program called the Childhood Cancer Data Initiative (CCDI), which has been funded at $50 million per fiscal year since 2020. Source: Cancer.gov
The Childhood Cancer Survivorship, Treatment, Access, and Research (STAR) Act is also funded; for FY 2024, NCI’s “funds available” included $28 million for STAR. Source: Cancer.gov
In FY 2024, the total NCI budget was about $7.2 billion, of which the CCDI and STAR Act portions are specific earmarks for childhood cancer research and survivorship. Source: Cancer.gov
Only between 4-8% of federal funding is allocated to childhood cancer research. Source: https://childrenscancerfoundation.org/why-we-do-it/statistics/